Sandpiper Launches AI Services for Communications and Public Affairs

Carbon Capture, Utilisation and Storage (CCUS) in China
Australian Budget 2023: Wins, Losses and What It All Means for Health
May 2023

By Eddie Morton, Associate Director of Sandpiper Health based in Australia. Eddie is a former journalist with extensive experience in healthcare PR and communications, specifically stakeholder and government relations, policy, advocacy, healthcare supply data analysis and communications
The Australian Government’s focus on health in the recent Budget was welcomed almost universally. Allocations for increased primary care access, multidisciplinary team-based care, technology, medicines and data sharing were all widely supported. But concerns remain about demand, fit-for-purpose rebates and rebate indexation and right-sited care (virtual or in-person). And while government promises are positive, the aged care sector is also awaiting the implementation of recommendations from the Royal Commission into Aged Care Quality and Safety.
Australians prioritise health like few others
Sandpiper’s Healthcare Tracker research consistently reveals Australia’s steadfast public support for its healthcare system.
Compared to their Asia Pacific neighbours, Australians place healthcare costs, quality and access above economy, jobs and the environment consistently. Their appreciation for their universal Medicare system – and its uniquely mixed private counterpart – consistently delivers high satisfaction levels. General practitioners, meanwhile, lead consumer sentiment scores, which is testament to the widely regarded GP-patient relationship in the face of intensifying demand.
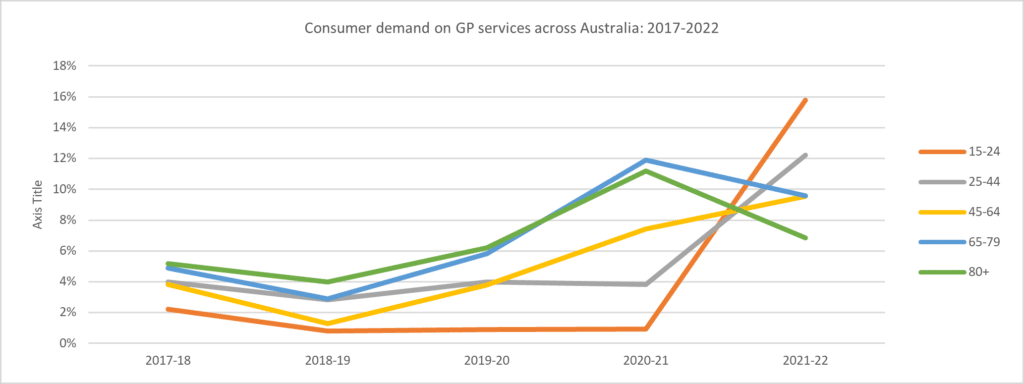
Australians are most concerned with the burden of cancer and chronic illness, the rise of mental conditions – especially among younger cohorts whose reliance on GP services is rapidly rising – and the threat of another pandemic. In response to these concerns, they want to seem more investment in health infrastructure, preventative health and affordable care.
| Which health condition are Australians most concerned about? |
|---|
| 1. Cancer |
| 2. Mental Illness |
| 3. Potential infectious disease outbreaks |
| What Australians want the government to spend money on? |
|---|
| 1. Hospitals & infrastructure |
| 2. Prevention of ill health |
| 3. Affordable care |
Medicare, however – the country’s much-adored universal health benefits scheme – is now 40 years old but has not kept pace with changes to population health and the cost of care.
The response, which this year’s Budget sought to relay: A decades overdue overhaul, which Health Minister Mark Butler forewarned as not going to be quick, not going to be easy and not going to be fixed in one budget.
The healthcare industry wanted drastic change in this year’s Budget
Ahead of the budget, Australia’s peak healthcare organisations urged greater funding for primary care to ease an accessibility crisis crippling the frontline community service and exacerbating accessibility, workforce and affordability issues down the line into tertiary (hospital) settings.
The AMA called for increased funding, improved indexation, and voluntary patient enrollment for GP services. The Pharmacy Guild proposed reduced co-payments, reformed indexation, and opposed 60-day dispensing. The ADA prioritised a Senior Dental Benefits Scheme, enhanced Child Dental Benefit Schedule, and improved funding for adult dental services.
PHA focused on combating fraud, reducing over-pricing of medical devices, abolishing second-tier benefits, and increasing the Medicare Levy Surcharge and Private Health Insurance Rebate. ACCPA requested more funding for Home Care Packages, addressing workforce shortages, and extending student visa holders’ working hours. CHA proposed increased consumer contributions, deregulation of the Basic Daily Fee, and an aged care innovation fund.
Vision 2020 Australia aimed to address vision loss, focusing on Aboriginal and Torres Strait Islander communities, publicly funded eye care, and research investment. AAMRI emphasized retaining researchers and increasing funding for research costs through Ideas Grants.
Budget 2023-24 breakdown for healthcare
Did industry get what they wanted? More than AUD$27.9 billion of new investments into health and aged care were announced. The centerpiece, according to Health Minister Mark Butler, was a tripling of the provision of bulk billing services for GPs and a 15% pay increase for all aged care workers.
For Primary Care
- The $5.7 billion Strengthening Medicare initiative includes measures to prevent the decline in GP bulk billing. This includes:
- $445.1 million for GPs to have nurses and allied health professionals working with them in cooperation for better care
- $143.9 million to encourage GPs to stay open for longer hours
- $98.9 million to connect frequent hospital users to general practices to multidisciplinary care
- $79.4 million to support primary health networks to commission allied health services to improve access to multidisciplinary care for people with chronic conditions in under-serviced communities
- Additional funding for after-hours programs, treatment of frequent hospital users by GPs, improved access for those with chronic health conditions, a wounds consumable scheme in general practice, the Royal Flying Doctors Service, and primary care clinical placements.
- $29.8 million for a Medicare fraud crackdown
- $824.4 million on digital health initiatives, including to modernise My Health Record
- What’s missing? Mental health did not get a mention in this year’s accounts, triggering frustration from the Royal Australian and New Zealand College of Psychiatrists who labelled the measures as “heavily weighted to wellbeing initiatives and primary care” and missing the opportunity to address care for severe, complex, and chronic mental health conditions. Additionally, the discontinuation of the Better Access mental health program – which increased public funded mental health visits to 20 sessions – also prompted criticism from industry.
For medicines
- The Seventh Community Pharmacy Agreement receives $654.9 million in funding, while $114 million is allocated to the National Immunisation Program.
- Increases to the maximum dispensing quantities allowed for more than 300 PBS-listed medicines, allowing for two-month prescription refills. This is projected to save Australians around $1.6 billion in out-of-pocket costs over the next four years.
- $79.5 million to support regional pharmacies affected by reduced income.
- $2.2 billion in funding for new and amended PBS listings.
- What’s missing? The government entirely scrapped the Patent Box initiative first put forward by the former Morrison Government in its 2021–22 Budget. The plan was to introduce a patent box that would tax corporate income derived from eligible Australian patents in the medical and biotechnology sectors, at a concessional rate of 17 per cent.
For wellbeing and allied health
- $141.2 million for the expansion of smoking prevention programs, $63.4 million for prevention and reduction, and $29.5 million for quitting programs.
- Tobacco excise increased, generating approximately $3.3 billion in revenue over the forward estimates, with $290 million distributed to the states as GST.
- $219.4 million to advance long-term adult public dental funding reform and extend funding for Public Dental Services for Adults until June 2025.
- $263.8 million for a new national lung cancer screening program
- $91.1 million on the establishment of the Australian Centre for Disease Control.
- A reallocation of $1.7 billion toward in-home aged care, home care packages, a 15% pay increase for aged care workers, and GPs in Aged Care.
For medical technology
- $40 million to establish the National Clinical Quality Registry Program for tracking the safety and performance of treatments and medical devices.
- $29.5 million to design, implement and maintain a range of cost recovery arrangements, including $11.4 million over 4 years (and $3.4 million ongoing) to fund enhanced services to the medical device industry under new arrangements relating to the Prostheses List. These costs will be partially offset from increased revenue of $9.3 million over 4 years ($3.3 million ongoing) recovered from existing and new charges for services to the industry.
- $61 million over 4 years from 2023-24 for the TGA’s delivery of “public good activities”.
- $125.6 million to improve access to primary health care services and improve clinical practice, including $23.6 million for orthopaedic MBS items, $18.5 million for testing genetic variants in patients suspected of having either myeloid or lymphoid haematological malignancy, $16.8 million for EndoPredict gene expression profiling test to determine a patient’s risk of recurrent breast cancer, and $13.1 million to introduce genetic testing for hearing loss in children.
- $3.1 million to introduce testing for quantification of N-terminal pro B-type natriuretic peptide in patients with systemic sclerosis to assess the risk of pulmonary arterial hypertension.
- $2.2 million to amend selected MBS Plastic and Reconstructive Surgery items and hospital requirements in line with sector advice, and to ensure patient safety.
- $47.8 million to improve the treatment of chronic wounds by establishing a Chronic Wound Consumables Scheme for people with diabetes aged 65 and First Nations people aged 50 years and over to provide eligible people with subsidised wound consumables
- What’s missing? The Australian government cancelled the previous government’s $44 million plan for Artificial Intelligence and Digital Capability Centres, which were aimed at helping Australian businesses improve their AI skills, connect small and medium enterprises (SMEs) with AI equipment and tools, increase the adoption of AI technologies, provide training and support the development and commercialisation of AI products and services.
What it all means
This year will mark a notable milestone in Australia’s journey to bolster its already world-class health system. The focus on upstream services in primary care, improving access and affordability through bulk billing, strengthening the coalface against demand with workforce funding, and preventative measures against smoking, vapes and cancer screening, all bode well for a future-proofed system.
“With access to GP care getting more difficult for these patients due to increasing out of pocket costs, this targeted support is much needed and will make a real difference, especially in rural and regional areas,” AMA President Steve Robson said in the wake of the budget. “This will ease pressure on GPs and help make care more convenient and accessible for patients.”
Adjunct Prof Terry Slevin, CEO of the Public Health Association of Australia, said all eyes will be on the government’s commitment to the Australian Centre for Disease Control.
“2023 is a milestone for public health in Australia because it’s when the Australian Government will give birth to its promised Australian Centre for Disease Control,” he said.
“We have been clear that funding needs to be in the hundreds, not tens of millions of dollars. A well-resourced and funded ACDC is absolutely crucial to Australia’s ability to prepare for pandemics of the future, as well as tackling the growing threat of preventable disease in Australia.”
Medicines Australia CEO Liz de Somer rallied the praise, highlighting the need for innovating medicines and a comprehensive Health Technology Assessment review.
“Medicare and the PBS must evolve together, and the Government’s first major Health Technology Assessment (HTA) review in 30 years provides a critical opportunity to achieve long overdue PBS reform. Making our HTA ‘fit for the future’, to sit alongside Medicare, must now be our collaborative goal,” said Ms de Somer.